MENU
JUMP TO
See the YouTube Terms of Service and Google Privacy Policy
Delivering Behavioral Health
Police-Mental Health Collaboration (PMHC) strategies offer behavioral health care providers, at the state and local levels the opportunity to improve the coordination of services with their law enforcement partners. This coordination can lead to improved public health outcomes for people with behavioral health care needs who come into contact with law enforcement.
This section gives an overview of the role of behavioral health providers when treating and delivering services to people with behavioral health care needs who come in contact with law enforcement. It discusses the importance of behavioral health leadership and collaboration to the implementation and sustainability of an effective PMHC strategy and demonstrates the value a PMHC offers to behavioral health care providers. Additionally, the behavioral health section highlights important collaborative activities—such as information sharing, training, and performance measurement—that can positively impact the treatment and daily outcomes of people with behavioral health needs.
Value of the PMHC for Providers
Many people who have behavioral health care needs, particularly those who also have co-occurring mental health and substance use disorders, may come into contact with law enforcement during moments of crisis. However, when behavioral health care providers at the state and locals levels partner with law enforcement to use effective PMHC strategies, they have an opportunity to support sustained wellness for people with behavioral health care needs. When these PMHCs are implemented and sustained, behavioral health care providers can expect to see the following positive outcomes:
Additional Resources:
- The Crisis Intervention Team Model of Police Response to Mental Health Crises: A Primer for Mental Health Practitioners
- Law Enforcement Responses to People with Mental Illnesses: A Guide to Research-Informed Policy and Practice
- Crisis Intervention Teams - Facts & Benefits
Behavioral Health Care Provider’s Role
Behavioral health care providers play a variety of roles in efforts to improve outcomes for people with mental illnesses who come in contact with law enforcement. At each of the points of intersection described below, behavioral health care providers have the opportunity to evaluate needs, and engage individuals in appropriate behavioral health services and treatment options.
Fielding Initial Contacts:
The most common way for law enforcement to learn of people in crisis or in need of behavioral health assistance is when someone calls a 911 dispatch center requesting a police response. Some of these calls describe situations that clearly involve a person with behavioral health needs, but in many instances this is not apparent to the caller or the 911 call-taker. Gathering as much information about the nature of the call and the needs of individuals involved is a critical first step to facilitating an appropriate response by law enforcement and other emergency responders.
- Guidance for 911 Dispatch Centers – Behavioral health care providers can work with 911 dispatch centers to assist with training for key personnel and to develop succinct questions that call-takers and dispatchers can ask to determine if a call involves someone with a mental illness.
- Clinicians in 911 Dispatch Centers – A licensed clinician can also be co-located in a dispatch center to help identify and triage behavioral health calls for service that may, or may not, require a response by law enforcement or other first responders (i.e. emergency medical staff).
- Behavioral Health Hotlines and Warmlines – Staffed by clinicians, hotlines can provide support to people in a time of near-crisis. Warmlines are usually peer run and offer support in a time of distress in an effort to prevent crisis. In both scenarios, call-takers can provide the caller with behavioral health care resources appropriate to the caller’s needs. It is important for administrators of these call lines to develop procedures for when callers should be directed to call “911” on their own or when call-takers should transfer calls directly to a 911 center, if feasible.
For More Information:
Responding On Scene to Behavioral Health Calls for Service:
Identifying and engaging people with behavioral health needs in face-to-face encounters can require additional behavioral health expertise to assist in keeping officers, the individual, and bystanders safe. Even with significant specialized training, officers often face challenges when trying to manage an encounter with a person with behavioral health needs or when trying to deescalate a crisis situation. Behavioral health care providers can assist law enforcement on-scene with assessing the seriousness of symptoms and behaviors related to mental illness in several ways.
- Dedicated Phone Line for Law Enforcement – The behavioral health partner designates a phone line for use by law enforcement officers to obtain clinical guidance for interacting with an individual or to receive assistance determining the appropriate disposition and locating available behavioral health resources.
- Co-responder Model – A clinician is paired with a law enforcement officer to jointly respond to, manage, and deescalate calls for service, including screening the individual to determine an appropriate course of action.
- Mobile Crisis Model – Behavioral health professionals respond to calls for service at the request of law enforcement to help screen the individual and determine an appropriate disposition.
Determining an Appropriate Disposition for an Encounter:
Reaching an appropriate disposition for people with mental illnesses requires officers have suitable options to meet their complex needs. Ideally, a behavioral health care facility should be able to assume custodial responsibility of individuals to allow officers to return to service with minimal delay. Behavioral health care providers can assist law enforcement with evaluation and appropriate referrals in several ways
- Non-Crisis Diversion – In non-crisis situations, when officers suspect that mental illness is a factor in their contact with an individual, they can make a referral to a behavioral health care provider who would then assess the individual and identify community-based support and services as appropriate.
- Outpatient Facility: Outpatient behavioral health facilities can designate staff to be available to screen individuals brought by law enforcement and engage in treatment and recovery planning.
- Shelters: When law enforcement encounters an individual without adequate shelter—considered homeless—they often assist with accessing shelter, particularly in inclement weather. This is an opportunity for behavioral health care providers to engage an individual in supportive housing, behavioral health services, and other case management needs.
- Sobering and Detox Center: When law enforcement officers encounter an individual who is intoxicated, these specialized centers can provide a safe, supportive environment for people to become sober and eventually enroll in a rehabilitation program.
- Crisis Diversion – When there is a crisis situation that does not warrant an emergency room-based evaluation, officers should seek less restrictive alternatives than arrest. In these circumstances, a clinician would assess the individual and make a referral to the appropriate treatment necessary to help stabilize the individual’s mental health. After the crisis is resolved, the individual can participate in discharge planning and be connected to community-based programming in an effort to prevent further crises.
- Engagement/Diversion Facility: Engagement or diversion facilities are robust settings with an array of crisis (and non-crisis) programming easily accessible to law enforcement. Many operate 24-7, 365 days a year. Services can include a crisis stabilization unit, sobering room, and residential detox.
- Short-Term Crisis Residential/Respite Center: At the direction of a behavioral health provider, law enforcement can escort people in crisis to short-term crisis residential programs which provide intensive programming to stabilize the individual’s mental health status.
- Emergency Evaluations/Hospitalization – In some jurisdictions, community behavioral health care providers play key roles in responding to law enforcement requests for involuntary evaluations or directing officers to the appropriate facility where an evaluation can occur. Behavioral health care providers can determine whether the individual is a “danger to self or others” and inform the officer’s decision on whether civil or criminal measures can safely be employed. In those jurisdictions, behavioral health care providers work with law enforcement agencies and hospitals to develop policies and procedures that aim to expedite the process so officers can return to service as quickly as possible.
- At Arrest – Some communities employ data-matching, in which arrest information is sent to the behavioral health provider to match with active case logs so that behavioral health care providers are updated when a client is arrested. In other jurisdictions, detention centers and jails employ a clinician to facilitate pre-booking mental health screening. Alternatively, outpatient behavioral health providers can also designate a clinician to be available to screen people under law enforcement detention for behavioral health needs.
For More Information:
Reducing Repeated Contacts:
Known as high utilizers of emergency services, certain people with mental illnesses repeatedly cycle through the criminal justice and behavioral health care systems and have multiple contacts with both agencies. Law enforcement and behavioral health care providers can collaborate on planning to prevent further contact with the criminal justice system in several ways.
- Case Management – Behavioral health providers and law enforcement can collaborate on case management aimed at promoting recovery, maintaining wellness, and avoiding crisis. The team would assess the individual for behavioral health needs, make appropriate referrals, or encourage the return to treatment. When special populations are involved (e.g., homeless individuals, veterans, and people with substance use disorders), coordination with other service providers would be required to address complex needs.
- Mobile Outreach – Mobile outreach services are similar to the non-crisis version of mobile crisis. These non-crisis referrals to mobile outreach can come from law enforcement, behavioral health care providers, and family and friends, with the purpose of assessing the individual’s wellness and encouraging engagement in treatment before the individual has a crisis.
For More Information:
Collaboration Strategies
An effective PMHC requires continuous leadership support to ensure that core agreements amongst partners at the state and local level are implemented. Agreements form processes that are routinely reviewed so that they remain responsive to shifting jurisdictional needs.
Collaboration:
Successful PMHC strategies require coordination with law enforcement agencies at the executive and program manager levels. This coordination can take multiple forms such as establishing mutual goals and objectives and defining personnel roles and responsibilities. PMHCs can help behavioral health, and law enforcement partners reach an accord on how to implement policies consistently across organizations and promote safe on-scene responses, referrals and diversion, information sharing, training, and other aspects of the partnership. These topics and related procedures can also be memorialized through interagency agreements.
For More Information:
- Law Enforcement Responses to People with Mental Illness: A Guide to Research-Informed Policy and Practice
- Police-Mental Health Collaboration Programs: Checklist for Behavioral Health Leaders
Peer Support Specialist Bill Carruthers
“The collaboration between the peer workforce and law enforcement drastically improves the projected outcomes for those in our criminal justice systems. I think the goal for everyone is the recovery of the person involved. It might be for different reasons, but it still is the goal. How many officers said to me, ‘I don’t want to take you to jail, but I don’t have any choice?’ Peer support is another choice. Recovery is another choice.
Peer support exposes people to the truth, not just about the trouble that they are in, but about the avenue out. I can tell you about the way I got out. That is part of my specific role—to share my lived experience.”
--Bill Carruthers, Certified Peer Specialist, CEO of Recovery on Fire and Board Member, NAMI Georgia
Coordinated Practices
While law enforcement, behavioral health care, and state and local mental health agencies are complex and distinct systems, all share an important goal: the reduction of people with behavioral health care needs having repeated contact with the criminal justice system. To achieve this shared goal, coordinated practices such as sharing information, collaborative training, and data collection are essential.
Information Sharing:
Information sharing between law enforcement and behavioral health care providers can help identify people at risk of having frequent contact with the criminal justice system, ensuring those individuals are linked to community-based services, and maintaining continuity of care if someone is arrested. It is important to consult relevant federal and state laws when developing protocols and procedures for how to share information and to determine when consent or authorization is necessary.
- Crisis De-escalation – Behavioral health care providers often have at least some access to medical and behavioral health care information that can be used during a crisis situation, especially with the addition of county-wide and regional Health Information Exchanges (HIEs) in many local jurisdictions., A clinician with access to the individual’s records may be able to guide the officers to help deescalate a crisis and reach an appropriate disposition. This guidance can be made available on-scene or by phone consultation.
- Collaborative Meetings – Many jurisdictions have implemented criminal justice-behavioral health collaborative meetings to bring together practitioners from both systems to lawfully share information and identify and address the needs of people with mental illnesses who are prone to frequent contact with law enforcement.
- Person-Centered Tools – The use of person-centered tools, such as Psychiatric Advanced Directives (PADs), can allow the person’s experiences, perception of recovery needs, and preferences to be shared with the responding officer and considered in crisis prevention and planning.
For More Information:
Collaborative Training
To help each system better understand the perspectives and protocols of their counterparts, criminal justice and behavioral health care practitioners should coordinate with each other when developing and delivering training and educational programs. Involvement of individuals with behavioral health care needs in the training can be particularly effective.
- Curriculum development – Each system helps develop and refine the relevant content of the other’s curriculum, including goals and objectives, lesson plans, supporting literature to improve accuracy, and practicality; and
- Cross-systems training – This type of training allows staff from each agency to become familiar with the policies and practices of the other and can include both classroom and community instruction. One example might be the opportunity to shadow each other’s work by participating in ride-alongs with officers or observing a crisis hot-line.
For More Information:
Data Collection:
Collecting and analyzing data on program performance is necessary to making informed decisions on resource allocation, crisis response practices, and treatment and recovery planning. Data collection may require adjustments to intake forms and other data collection tools.
- Behavioral health care provider requests of law enforcement can include data measurements such as the number of contacts between a person with behavioral health care needs and law enforcement, frequency of contacts, who initiated the contact, the reason for contact, and the final disposition of the encounter (e.g. medical or psychiatric ER or other community-based crisis center arrest, left on scene with referral information, etc.).
- Law enforcement requests of behavioral health care providers can include data measurements such as the frequency and type of assistance requested from the partner agency, the reason for the contact (e.g. referral to services, information sharing, recovering planning/case management, etc.), and the circumstance of contact with a person with behavioral health care needs (e.g. period of overall stability, escalation, or crisis).
For More Information:
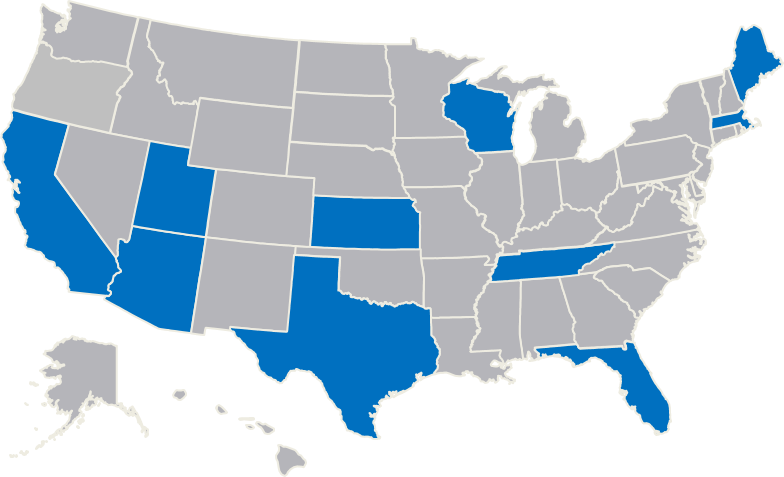
Law Enforcement-Mental Health Learning Sites
Support jurisdictions in exploring strategies to improve the outcomes of encounters between law enforcement and people who have mental illnesses.
Contact Police Mental Health Collaboration
Please submit questions, policies and training materials that can benefit others for review and consideration.
Focused Tools for Law Enforcement
Many communities struggle with the PMHC program design process. Communities are unsure how to design and develop a PMHC program that meets their distinct needs and challenges. One way to increase knowledge of PMHCs, is to review programs that other jurisdictions have developed and tailor those programs to your specific community needs.
Law Enforcement agencies interested in expanding their knowledge base, starting, or enhancing a PMHC, can contact The U.S. Department of Justice’s Bureau of Justice Assistance (BJA) or BJA’s Training and Technical Assistance (TTA) Provider. BJA supports these urban and rural police departments to act as host-sites to visiting law enforcement agencies and their mental health partners.
- Arlington (MA) Police Department
- Bexar County (TX) Sheriff's Office
- Harris County (TX) Sheriff's Department
- Houston (TX) Police Department
- Los Angeles (CA) Police Department
- Madison County (TN) Sheriff's Office
- Madison (WI) Police Department
- Miami-Dade County (FL) Police Department
- Portland (ME) Police Department
- Salt Lake City (UT) Police Department
- Tucson (AZ) Police Department
- University of Florida Police Department
- Wichita (KS) Police Department
- Yavapai County (AZ) Justice & Mental Health Coalition
Located across the country, these learning sites represent a diverse cross-section of perspectives and program examples and are dedicated to helping other jurisdictions improve their responses to people with mental illnesses.
Opportunities
The fourteen learning sites host site visits from interested colleagues and other local and state government officials, answer questions from the field, and work with BJA’s TTA provider to develop materials for practitioners and their community partners.
TTA is provided to law enforcement agencies and their community partners in an effort to assist with the development or implementation of PMHC strategies. Supplemental funds can be made available to agencies that are interested in visiting the learning sites. This is a focused approach intended to provide your agency with access to outstanding peer resources for police-mental health collaboration programs.
To request TTA and receive confirmation within 36 hours of your request
Complete the TA request form.
For questions not addressed by the Law Enforcement Mental Health Learning Site web page, contact [email protected]