MENU
JUMP TO
Managing Police-Mental Health Collaborations
See the YouTube Terms of Service and Google Privacy Policy
A comprehensive PMHC program affects several different law enforcement functions. Many agencies designate an individual to be the program manager or coordinator. The program manager’s role requires a person with targeted experience and knowledge to coordinate the diverse components of the PMHC program. For smaller agencies, the program manager’s role can be collateral duty. In other agencies, it may be a part-time or a full-time position. Some of the nation’s mid-sized and larger agencies have established organizational units or divisions to demonstrate that the PMHC program is an agency priority. This also allows the agency to enhance program coordination and oversight.
This section provides an overview of the agency functions that play a key role in ensuring the success of the PMHC program, including:
- Policies and Procedures
- Call-taking and dispatching procedures
- Protocols to divert individuals from the criminal justice system
- Partnership agreements with mental health providers
- Information-sharing protocols
Sharing Program Management with Community Partners
PMHCs benefit when law enforcement collaborates with, and are inclusive of, mental health service delivery partners and mental health advocates—including people living with mental illnesses and their families. Including community organizations and advocates as partners raises awareness of program successes and enhances community trust in the program. These partners can also help sustain the program over the long term by seeking funding opportunities, cultivating champions or educating elected officials. Ensure these stakeholders are engaged as equal partners in your taskforce or steering committee.
Learn more:
- Sharing Management of Police-Mental Health Collaborations (PMHCs): The Benefits of Partnering with People with Mental Illness, Families and Advocates
Policies and Procedures
Written policies and procedures play an important role in the overall management and success of a PMHC program. They provide law enforcement agency employees with a clear understanding of the PMHC program by:
- Affirming agency principles.
- Delineating procedures for carrying out program activities.
- Providing critical information for working with mental health partners.
Some agencies use one written directive for the entire program, while others reference the PMHC program in several, relevant directives.
- Download the Law Enforcement Program Manager’s Checklist for guidance
- Stabilization, Observation, and Disposition Essential Element
- Organizational Support Essential Element
Examples of Policies
Call Taking and Dispatching
Call takers and dispatchers are key partners in the successful management and coordination of a PMHC program. 911 emergency dispatch centers are often the first point of contact for mental health calls for service. Determining that mental illness is a factor in a call for service is an essential first step to providing appropriate police response. To facilitate coordination between the PMHC program and dispatch center, many agencies have developed protocols and specific questions to aid call takers and dispatchers gather critical information, which is then conveyed to the officers. This is essential for officer safety and will allow for consideration of the most appropriate response.
For More Information:
Community-based Resources
Community-based mental health resources and services play key roles in the operations and success of PMHC programs by offering immediate alternatives to incarceration for people with mental illness. To that end, many communities are establishing crisis care centers, which reduce overreliance on both jail and hospital emergency rooms and allow officers to return to service in a timely manner.
Carefully cultivating and managing relationships with mental health care providers ensure that officers are aware of these resources and use them in accordance with rules and admission criteria.
For more information:
See the YouTube Terms of Service and Google Privacy Policy
Partnership Agreements
The success of these programs often rests on the ability of law enforcement and mental health agencies to effectively work together. Interagency agreements, such as memorandums of understanding (MOUs) are effective mechanisms to:
- Delineate role and responsibilities
- Identify resources to be contributed
- Document joint policies and procedures
One of the challenges to collaboration is sharing an individual’s information between law enforcement and mental health providers. However, this can be addressed through an agreement such as a memorandum of understanding or an information-sharing agreement, or another type of interagency agreement. What is of critical importance, is that collaborating partners have a clear understanding of what information can and cannot be shared. The agreed-upon protocols should then be documented within the partnership agreement.
Examples of Collaborative Agreements; MOUs, DUAs, BAAs, and more
Information Sharing
Many jurisdictions have developed strategies to facilitate appropriate information sharing among behavioral health and law enforcement agencies. The following tips are based on their experiences:
- Effective collaboration builds on cooperation and trust between agencies.
- It is possible to share information legally.
- Remember the principle of sharing the minimum necessary health information.
- Think about engaging people with lived experiences in establishing strategies.
Additional Resources
- Information Sharing between Mental Health and Criminal Justice Agencies
- Team Planning for Data-Driven Justice
- Information Sharing in Criminal Justice-Mental health Collaborations
- Information Exchange and Confidentiality Essential Elements
- Sharing Behavioral Health Information: Tips
- A Guide for Family Educational Rights and Privacy Act
FAQs
Managing
Law Enforcement-Mental Health Learning Sites
Support jurisdictions in exploring strategies to improve the outcomes of encounters between law enforcement and people who have mental illnesses.
Contact Police Mental Health Collaboration
Please submit questions, policies and training materials that can benefit others for review and consideration.
Focused Tools for Law Enforcement
Many communities struggle with the PMHC program design process. Communities are unsure how to design and develop a PMHC program that meets their distinct needs and challenges. One way to increase knowledge of PMHCs, is to review programs that other jurisdictions have developed and tailor those programs to your specific community needs.
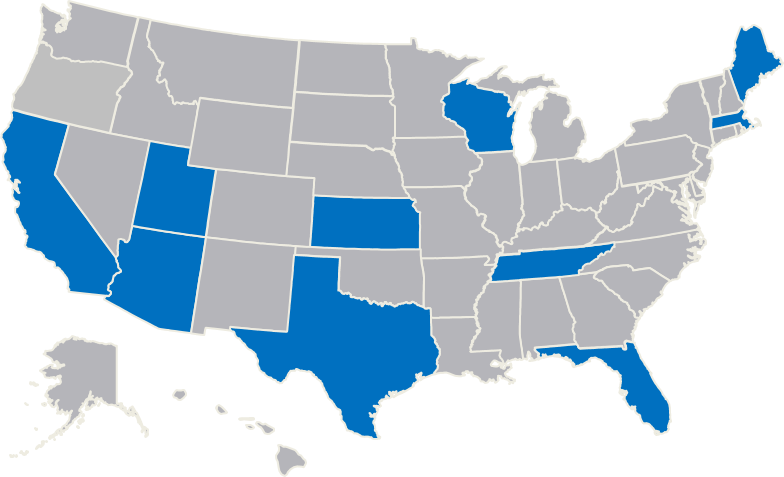
Law Enforcement agencies interested in expanding their knowledge base, starting, or enhancing a PMHC, can contact The U.S. Department of Justice’s Bureau of Justice Assistance (BJA) or BJA’s Training and Technical Assistance (TTA) Provider. BJA supports these urban and rural police departments to act as host-sites to visiting law enforcement agencies and their mental health partners.
- Arlington (MA) Police Department
- Bexar County (TX) Sheriff's Office
- Harris County (TX) Sheriff's Department
- Houston (TX) Police Department
- Los Angeles (CA) Police Department
- Madison County (TN) Sheriff's Office
- Madison (WI) Police Department
- Miami-Dade County (FL) Police Department
- Portland (ME) Police Department
- Salt Lake City (UT) Police Department
- Tucson (AZ) Police Department
- University of Florida Police Department
- Wichita (KS) Police Department
- Yavapai County (AZ) Justice & Mental Health Coalition
Located across the country, these learning sites represent a diverse cross-section of perspectives and program examples and are dedicated to helping other jurisdictions improve their responses to people with mental illnesses.
Opportunities
The fourteen learning sites host site visits from interested colleagues and other local and state government officials, answer questions from the field, and work with BJA’s TTA provider to develop materials for practitioners and their community partners.
TTA is provided to law enforcement agencies and their community partners in an effort to assist with the development or implementation of PMHC strategies. Supplemental funds can be made available to agencies that are interested in visiting the learning sites. This is a focused approach intended to provide your agency with access to outstanding peer resources for police-mental health collaboration programs.
To request TTA and receive confirmation within 36 hours of your request
Complete the TA request form.
For questions not addressed by the Law Enforcement Mental Health Learning Site web page, contact [email protected]