MENU
JUMP TO
Planning and Implementing a Police-Mental Health Collaboration Program
See the YouTube Terms of Service and Google Privacy Policy
Effective PMHC programs share a common adherence to the essential elements, but they also differ in some important ways resulting from the variations generally stemming from a community’s needs, resources and limitations. To develop the appropriate type of PMHC program, each community should embark on a planning and discovery process that reflects their unique characteristics.
This section provides an overview of planning and implementing a PMHC program. It focuses on the importance of leadership by chiefs and sheriffs, working collaboratively with mental health and community stakeholders, and a using a multi-step program design process.
Leadership Matters
Strong leadership is essential for planning and implementing a PMHC program. Law enforcement leaders, chiefs, sheriffs, and directors must make the PMHC program a priority in their own agencies; ensuring qualified personnel and resources are in place to support the planning and implementation process.
What if law enforcement officers need information regarding officer health and wellness?
Chiefs and sheriffs are in unique positions to provide leadership for a collaborative approach that includes engaging other community stakeholders to ensure effective planning and implementation of a PMHC program. They have the ability to convene other, external leaders with operational decision-making authority from each of the stakeholder agencies, as well as community representatives to form a multidisciplinary executive-level planning committee. This committee would be charged to examine the local challenges and determine the program’s goal, objectives, and design to ensure its development and continuity.
Agency leaders on the planning committee must designate appropriate staff to comprise a program coordination group, which would be responsible for overseeing the day-to-day activities. In some jurisdictions, the two bodies may be the same—particularly those with small agencies, in rural areas, or with limited resources.
Leadership:
Strong support from the behavioral health care agency executive and management staff is essential to a successful PMHC. This support requires a continuous recognition from the director and executive-level staff that the collaboration is an agency priority and is critical to the agency’s mission. When successful, leadership assigns qualified personnel and resources to the PMHC including a designated manager to oversee the operations and serve as the liaison between behavioral health care services, and law enforcement. Champions from the board of directors may also further reinforce these efforts by advocating for the agency’s ongoing commitment to the PMHC and influencing how resources and funds are allocated.
For More Information:
Partnering with People with Mental Illness and Family Members
People living with mental illness, their family members and advocates are essential partners in police mental health collaborations at every step of program design and implementation. These stakeholders have been directly affected by the mental health crises, and can provide insight into how law enforcement interactions are experienced by the people in crisis and offer ways to improve response. People with mental illnesses and their families can share first-hand learning during PMHC training by sharing their personal experiences. Last, mental health advocates are experts at building relationships and advocating for needed mental health services.
Stakeholders
Meeting the challenges associated with police response to people with mental illnesses requires the commitment and participation of many community stakeholders. Stakeholders are those people or entities who are affected, or could be affected, by the service being provided. Stakeholders are individuals, groups, organizations, government departments, and businesses, anyone with a stake or a vested interest in improving responses to people with mental illnesses. They play critical roles in identifying resources and strategies for a PMHC program.
Local partners for the law enforcement agency should include:
- Mental health service providers
- Mental health consumers and their family members and loved ones
- Mental health advocates, such as NAMI
- Other area law enforcement professionals
- Substance abuse treatment providers
- Homeless advocates and housing officials
- Hospital and emergency room administrators
- Other criminal justice personnel such as prosecutors and jail administrators
- Elected officials
- State, local, and private funders
- Community members
In addition to local stakeholders, national-level organizations and associations, such as the National Alliance on Mental Illness (NAMI) and the National Council on Behavioral Health, provide guidance and resources, which can be adapted to each community.
National Behavioral Health and Criminal Justice Organizations
Here is list of national organizations with resources and materials for PMHC programs
Program Design and Implementation
The PMHC program design must be specific to the unique characteristics of the community being served. Each location is characterized by different people, cultures, skills and resources, and the best approach takes these characteristics into consideration. In addition, the program design must be guided by the problem (as described by consumers, committee members or provided credible data sources) in that jurisdiction. There is no “one-size-fits-all” approach that will work in every community.
Further, it is vital that the leaders in law enforcement, mental health, and consumer advocacy understand what obstacles they must overcome to outline steps for the development and success of an appropriate and effective PMHC program. Also, it is important to identify those agency strengths and resources that can address and overcome the identified obstacles.
The key steps to consider are listed here. For a more detailed discussion please see: “Improving Responses to People with Mental Illnesses: Tailoring Law Enforcement Initiatives to Individual Jurisdictions.”
Checklist of Key Steps for Planning, Designing, and Implementing a Police-Mental Health Collaboration Program
Step 1: Understand the problem
- What environmental and community forces are driving current efforts to improve the law enforcement response to people with mental illnesses?
- What data can the planning committee members examine to understand the factors influencing law enforcement responses to people with mental illnesses? Refer to Police-Mental Health Collaborations: Implementing Effective Law Enforcement Responses for People Who Have Mental Health Needs for guidance on collecting and analyzing data for PMHCs.
- What concerns have been raised by people living with mental illnesses, family members and mental health advocates?
Step 2: Articulate program goals and objectives
- What are the program’s overarching goals?
- What are the program’s objectives?
- How will the program serve people experiencing mental illness in your community?
- How will the program support public safety?
- How will program development include community perspectives and buy-in?
Step 3: Detail jurisdictional characteristics and their influence on program responses
- What law enforcement agency resources are relevant in planning a PMHC program?
- What mental health system resources are relevant in planning a PMHC program?
- What resources do mental health advocacy organizations have to offer in planning a PMHC program?
- What information is available from trained peer specialists familiar with your local social service system and criminal justice system?
- What state laws are relevant in planning a PMHC program?
- What demographic and geographic community considerations are relevant in planning a PMHC program?
Step 4: Establish response protocols
- What law enforcement responses are necessary?
- What mental health system responses are necessary?
- How can related agencies, such as emergency communications and emergency medical services support your response?
- Can mental health peer specialists be integrated into your crisis response?
- What other responses or resources are necessary?
Step 5: Determine training requirements
- How many hours of training will be provided?
- Who will receive this training?
- What topics will the training cover?
- Who will provide the training?
- What training strategies will be employed?
- What curriculum will be used for the training?
- How will mental health advocates participate in training development?
- How will trainees interact with people living with mental illness and their family members during training?
Step 6: Identify data-collection procedures to track performance
- What data will be collected to measure whether goals and objectives have been achieved?
What data collection strategies will be used?
- How will data collection capture whether people living with mental illness and their family members are satisfied with outcomes of the program?
- How will data collection capture information about outcomes for the individual in crisis (e.g., whether the person received treatment, whether the person was arrested)?
- Who will be responsible for the measuring performance?
- How will the evaluation be used to make improvements to the program?
- What resources and partnerships are needed to objectively collect and analyze data?
See the YouTube Terms of Service and Google Privacy Policy
Agency Experiences
This is What Community Policing Looks Like
A team in the Houston Police Department is trying something new when addressing complaints associated with people living on the streets.
Resources
An Integrated Approach to De-Escalation and Minimizing Use of Force
ICAT Training Guide Materials
- ICAT: Integrating Communications, Assessment, and Tactics – Developed by the Police Executive Research Forum and reviewed by policing experts across the country, this training guide delves into critical decision making, crisis recognition, tactical communications, operational safety, and integration of these practices into department’s standard operating procedures.
- Informed Police Responses Products – The webinars, presentations, written resources, and best practice guide for law enforcement were developed via the Academic Training Initiative and are designed to provide much needing information and training to law enforcement agencies and their partners who are developing new crisis response programs.
- Dirigo Safety's Online Courses – The online/in person courses developed and provided by Dirigo Safety cover a multitude of topics: from law enforcement response to mental health calls, to implicit human bias, to wellness and resiliency for law enforcement.
- CIT International's Best Practice Guide – CIT International, a leading voice in training law enforcement officers for crisis situations, published this highly comprehensive guide to assist departments around the country in developing their own training programs.
- Mental Health First Aid – Developed by the National Council on Mental Wellbeing, Mental Health First Aid is a course that teaches participants to identify and respond to a person who is experiencing a mental health crisis or developing a mental health problem. They offer adult and youth specific courses, as well as classes to become a trainer, which empowers participants to then turn around and teach others about these subjects.
- GAINS Center: Trauma Training for Criminal Justice Professionals – Sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA), the Gains Center provides training on a number of subjects. Trauma training for criminal justice professionals is one that is of particular importance for PMHCs. Train the trainer programs are available in addition to the standard training course.
FAQs
Planning and Implementing PMHCs
Law Enforcement-Mental Health Learning Sites
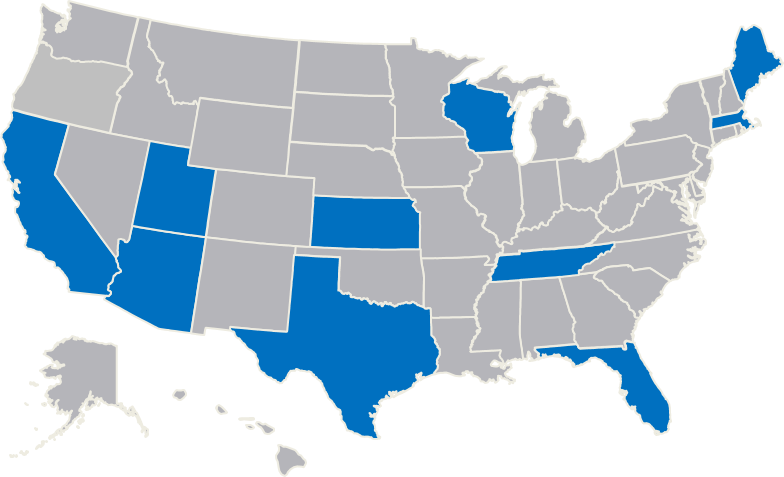
Support jurisdictions in exploring strategies to improve the outcomes of encounters between law enforcement and people who have mental illnesses.
Contact Police Mental Health Collaboration
Please submit questions, policies and training materials that can benefit others for review and consideration.
Focused Tools for Law Enforcement
Many communities struggle with the PMHC program design process. Communities are unsure how to design and develop a PMHC program that meets their distinct needs and challenges. One way to increase knowledge of PMHCs, is to review programs that other jurisdictions have developed and tailor those programs to your specific community needs.
Law Enforcement agencies interested in expanding their knowledge base, starting, or enhancing a PMHC, can contact The U.S. Department of Justice’s Bureau of Justice Assistance (BJA) or BJA’s Training and Technical Assistance (TTA) Provider. BJA supports these urban and rural police departments to act as host-sites to visiting law enforcement agencies and their mental health partners.
- Arlington (MA) Police Department
- Bexar County (TX) Sheriff's Office
- Harris County (TX) Sheriff's Department
- Houston (TX) Police Department
- Los Angeles (CA) Police Department
- Madison County (TN) Sheriff's Office
- Madison (WI) Police Department
- Miami-Dade County (FL) Police Department
- Portland (ME) Police Department
- Salt Lake City (UT) Police Department
- Tucson (AZ) Police Department
- University of Florida Police Department
- Wichita (KS) Police Department
- Yavapai County (AZ) Justice & Mental Health Coalition
Located across the country, these learning sites represent a diverse cross-section of perspectives and program examples and are dedicated to helping other jurisdictions improve their responses to people with mental illnesses.
Opportunities
The fourteen learning sites host site visits from interested colleagues and other local and state government officials, answer questions from the field, and work with BJA’s TTA provider to develop materials for practitioners and their community partners.
TTA is provided to law enforcement agencies and their community partners in an effort to assist with the development or implementation of PMHC strategies. Supplemental funds can be made available to agencies that are interested in visiting the learning sites. This is a focused approach intended to provide your agency with access to outstanding peer resources for police-mental health collaboration programs.
To request TTA and receive confirmation within 36 hours of your request
Complete the TA request form.
For questions not addressed by the Law Enforcement Mental Health Learning Site web page, contact [email protected]